At Cancer Starts With Can, we are dedicated to providing you with resources, support, and a community you can rely on.

Grants life-changing wishes for kids with critical illnesses (generally ages 2½–18), working with each child’s medical team to time wishes safely. Wishes can be referred by families, clinicians, or even the kids themselves and are fulfilled across the U.S. and beyond.

Regional, hands-on support for families of children with cancer—financial assistance, practical help during treatment, and community programming. If you’re in CT/Westchester, this is a great local group to rely on.
Beyond funding research, ALSF runs direct family services like Travel For Care (help with transportation/lodging to treatment) and programs for siblings and survivors. Families can apply online and tap into webinars and community stories.

Free/low-cost “home-away-from-home” lodging near hospitals so families can stay close to their child; many locations also offer Family Rooms inside hospitals and mobile care units. Find and contact your nearest House chapter right from their site.
Nationwide parent-founded nonprofit offering free educational materials, advocacy, and family support programs; they also help connect families to resources in their state. (They were formerly “Candlelighters.”)

A national network (and online platform) offering free support groups, individual counseling, educational workshops, and a toll-free Helpline (available in English & Spanish). Search by zip code for local CSC or Gilda’s Club locations.

Provides Transportation Assistance for travel/lodging to treatment, emergency aid, free publications for parents, and Beyond the Cure resources (including scholarships) for survivors. Families can apply and talk to a parent advocate.

Helps families manage the financial side of a pediatric cancer diagnosis with grants, resource navigation, and budgeting coaching—aimed at keeping housing, transportation, and basic needs stable during treatment. You can request support directly.
.png)
A powerful targeted therapy called Larotrectinib shrank a 44 cm tumor in a 3-month-old baby to nearly nothing within five weeks—with no side effects. A striking example of precision medicine at work.
.png)
Trials in England revealed that whole genome sequencing can deliver faster, more accurate cancer diagnosis and treatment plans for children—sometimes in just 10 days—while also identifying inherited risk factors for families.
.png)
CAR T-cell therapy—an advanced immune-based cancer treatment—has helped children beat leukemia. A biotech startup is now automating its production to make this life-saving therapy more affordable and widely available.
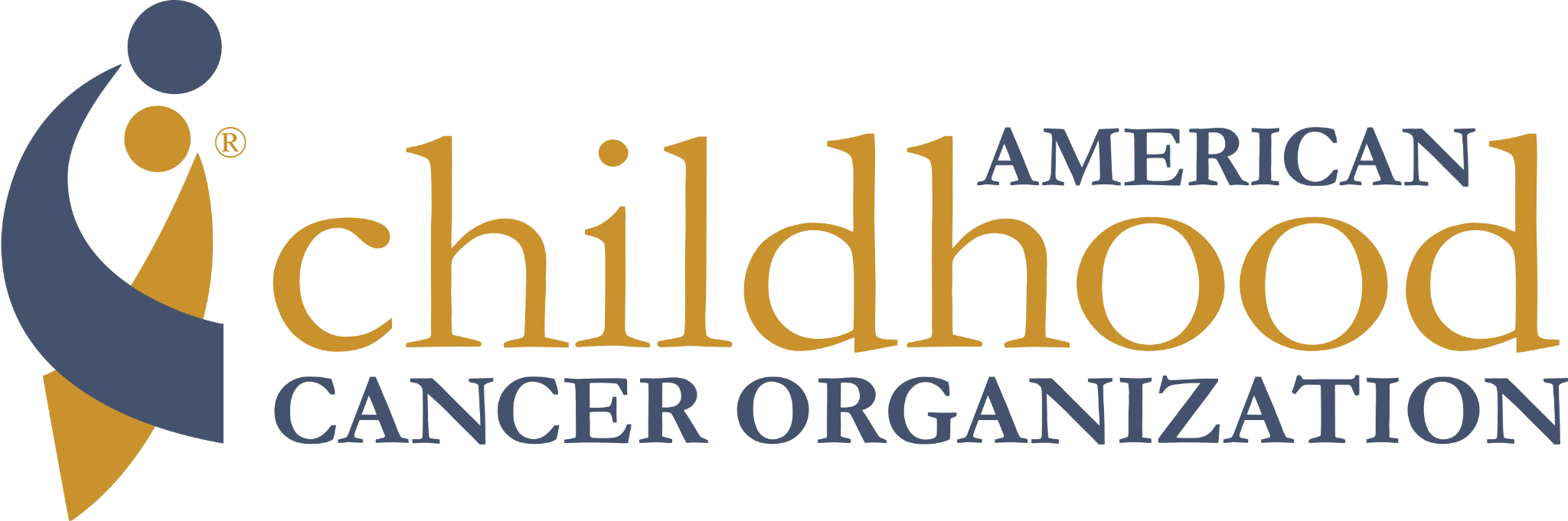
More kids are surviving cancer than ever—but many face long-term effects like fertility issues, heart and organ damage, or emotional challenges. New research emphasizes the importance of survivorship care plans, like the “Passport for Care,” to help children thrive.
.png)
Researchers from Emory University and QIMR Berghofer have developed a promising drug called CT‑179 that targets stubborn tumor cells in medulloblastoma—a common and aggressive pediatric brain cancer. In early mouse models, CT‑179 not only reaches and kills those dangerous cells but also boosts the power of radiation treatment, offering a potentially more effective and less toxic therapy option.
.png)
Researchers have developed a promising "universal" mRNA cancer vaccine that primes the immune system to fight multiple cancer types—including pediatric brain cancers and bone tumors—without the delay of personalized manufacturing. It’s now entering human trials for high-grade pediatric glioma and osteosarcoma, with hopes of transforming how childhood cancers are treated.